Why EHRs Fail to Deliver ROI
EHR implementations fall short of expectations for a variety of reasons, but, generally, they boil down to just a few key categories.
1.) Implementation Too Generic
Many health systems opt for implementing generic “foundation” or “model” systems based on recommendations from EHR vendors as a way to increase speed of deployment and decrease costs. Although this approach often does decrease overall program costs, it can also yield serious consequences. In a rush to get to implementation, little time and few resources are allocated to investigating and optimizing workflows and building the system to support the improvements.
2.) Lack of Formal Benefits Realization Program
For some organizations, EHR implementation took place long enough ago that value-based payment models — and the role their EHRs would play in enabling improved value — weren’t even on the radar. Now facing extensive optimization requests to meet regulatory requirements, many health systems do not have a formal benefits realization program or the appropriate governance in place to decide which projects to tackle.
3.) Pulling Resources or Measuring Results Too Soon
Finally, many organizations commit resources to optimizing workflows and using technology to enable the workflows as a part of implementation — but stop there. Benefits take time to realize, in some cases years. If work on benefits realization ceases when implementation is complete, or final measurements are taken too soon after go-live to determine if ROI has been achieved, the result is often significant disappointment.
How to Maximize EHR ROI
It’s never too late to optimize and generate value from the EHR. To achieve benefits through EHR optimization, health systems must do two things:
1.) Select high-value optimization targets that are aligned with organizational goals
2.) Utilize a comprehensive approach to performance improvement that focuses on opportunity identification, root cause analysis, and “speed-to-value” benefit delivery.
Impact Advisors’ Revenue Cycle Improvement Model is an agile-based multidisciplinary approach that delivers both cash acceleration and margin improvement through the alignment of process workflows and system functionality designed for maximized performance. Utilizing a series of “sprints” over a 6-to-9-month period focused on post-live optimization and Revenue Cycle improvement, Impact Advisors develops a comprehensive set of initiatives aimed at evaluating people, processes, and technology, achieving improvements in performance, adopting industry best practices, and maximizing investment.
Post-Live Optimization Activities
- Resolution of system and workflow break/fixes
- Analysis and optimization of workqueue logic
- Assignment of accountable owners for workqueues
- Improved understanding of performance dashboards
- Development of metric-based action plans
- Creation and/or standardization of processes
Revenue Cycle Improvement Initiatives
- Reduction in Candidate for Billing (CFB) Days
- Reduction in A/R Days
- Reduction in Open Denials
- Reduction in Write-offs
- Reduction in workqueue backlogs
- Increase in use of system automation
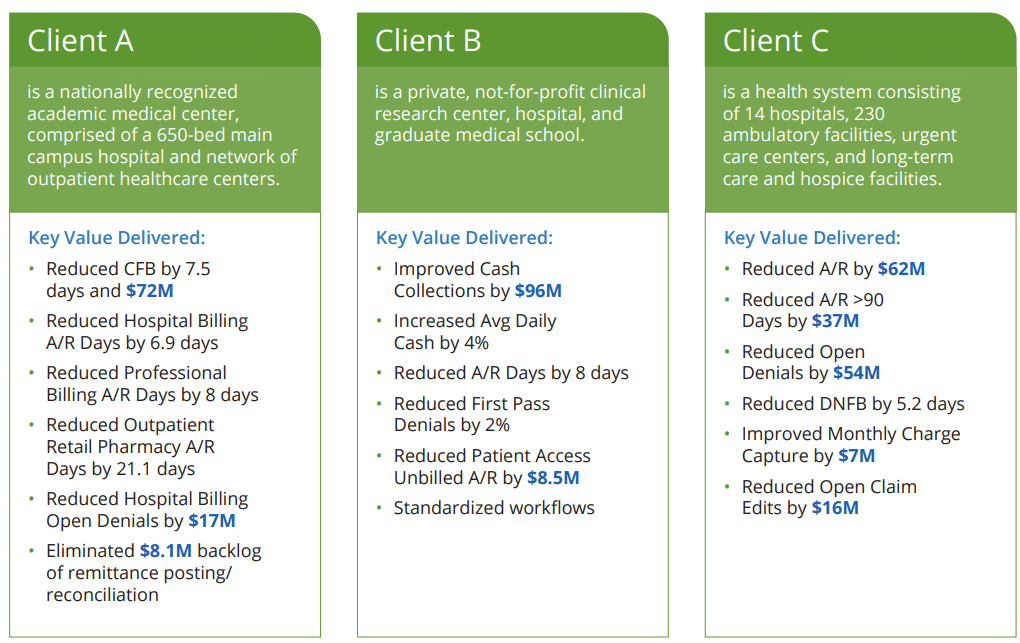
Our Client Impact