Over the past 20 years, the rate of survival for critically ill patients has dramatically improved. For some, however, survival has come at a cost. According to ICU Liberation co-founder Dr. W. Ely of Vanderbilt University, “For millions of new survivors comes new suffering and disability called Post-Intensive Care Syndrome (PICS). Patients with PICS are robbed of their normal cognitive, emotional, and physical capacity and cannot resume their previous life,” (2017). Impacting 25-75% of ICU survivors and 60-80% of COVID-19 survivors (Rawal & Kumar, 2021), the symptoms of PICS arise following critical illness and persist far beyond acute care hospitalization, resulting in pain, stress, and financial devastation to patients and families.
There is, however, hope. The evidence shows that implementation of the ICU Liberation Bundle can reduce, or eliminate the threat of PICS, improve patient outcomes, and reduce healthcare costs.
What is the ICU Liberation Bundle?
ICU Liberation is a bundle of care elements that should be applied to every patient in the intensive care unit (ICU) to liberate critically ill patients from the harmful effects of an ICU stay. The 2018 Clinical Practice Guidelines for the Prevention and Management of Pain, Agitation/Sedation, Delirium, Immobility and Sleep Disruption (Devlin et al., 2018) set the foundation for this bundle. Developed by the Society of Critical Care Medicine (SCCM) in collaboration with the American Association of Nurses (AACN) and supported by the Joint Commission, the ICU Liberation Bundle, also known as the A-F Bundle, consists of six elements that work synergistically to improve both short and long-term clinical outcomes, lessen critical care staff stress and burn out, and significantly lower the risk of PICS. By reducing ICU length of stay, shortening mechanical ventilator duration, and decreasing hospital readmissions, the ICU Liberation has also been shown to reduce healthcare costs and the capacity burdens imposed upon the healthcare system. Patients who were previously discharged to long term acute care centers or skilled nursing facilities can now return home – and back to their normal lives. Sadly, many hospitals have yet to implement this coordinated bundle of care.
The ICU Liberation Bundle includes the multidisciplinary development and implementation of policies, protocols, and interventions to address the following six elements:
A – Assess, Prevent, and Manage pain
B – Both Spontaneous Awakening Trials (SAT) and Spontaneous Breathing Trials (SBT)
C – Choice of Analgesia and Sedation
D – Delirium: Assess, Prevent, and Manage
E – Early Mobility and Exercise
F – Family Engagement and Empowerment
The ICU Liberation Bundle and Evidence-Based Outcomes
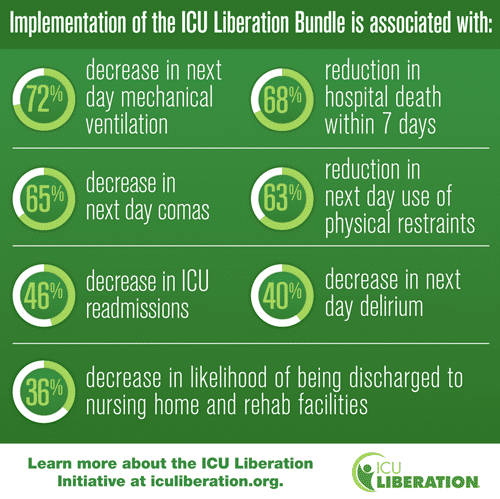
Evidence has repeatedly shown many benefits to bundle utilization in critical care units across the country. In 2018, the ICU Liberation Collaborative study, including more than 15,000 adult ICU patients from 68 academic, community, and federal ICUs found significant and clinically meaningful improvements in survival, mechanical ventilation use, coma, delirium, restraint-free care, ICU readmissions, and post-ICU discharge to skilled nursing or long-term acute care facilities. This study also demonstrated a dose related effect of the bundle, meaning that as more elements of the bundle are implemented in the patients’ care, the liklihood of positive outcomes grows (Pun, et al., 2018). Additionally, results of a study done in the 34 hospital Dignity Health System (now a part of CommonSpirit Health) revealed statistically significant reductions in ICU length of stay (LOS), mechanical ventilation duration, and long term (> 7 days) ICU stays for mechanically ventilated patients along with a reduction in hospital LOS. (J. Barr et al., 2024).
Evidence also supports financial incentives to bundle implementation. In their study, Fish et al., (2022) documented a $4.3 million hospital cost savings over a 5-year post implementation period based upon decreased LOS estimates. Dr. J. Barr of Palo Alto Health Care System in Palo Alto, California documented, “The net effect of our bundle implementation efforts in 2017 was to significantly reduce ICU and hospital length of stay which translates into a $6 million net cost savings to our facility, “(SCCM, 2019).
Utilization of the electronic health record (EHR) can aid in bundle compliance by creating a visual display of key performance indicators (KPIs)for clinicians implementing the bundle. Using role-based training throughout all ICUs in their hospital, monitoring and display of KPI’s on EHR enabled dashboards, Brown et al., (2022) were able to improve bundle compliance in their hospital. Clinicians from the University of Southern California’s eight-ICU tertiary care hospital also received real time and ongoing data literacy education to aid in dashboard interpretation. Like others before it, this study confirmed that bundle use resulted in lower next day ICU and hospital mortality rates, increased liklihood of next day extubation, and a higher number of patients being discharged home as opposed to a lower level of care (i.e., skilled nursing facilities, rehab facilities, or long-term acute care hospitals).
In February of 2020, Epic and Cerner (now Oracle Health) incorporated the ICU Liberation Bundle into their EHR software for both adult and pediatric patients. Patricia J. Posa, Quality and Patient Safety Program Manager for the Adult Hospitals at Michigan Medicine, stated “The adoption of the ICU Liberation Bundle in EHR systems is a game-changer for improving the care of the ICU patients. Following the evidence-based guidelines featured in the bundle has proven to reduce the liklihood of hospital death within seven days and cut readmissions in half, along with other improved patient outcomes. The challenge in ensuring the guidelines are adopted at all hospitals has been getting them in front of clinicians during the course of care. Inclusion of the bundle in an EHR is one of the most impactful ways to ensure they are implemented.” (Agency on Healthcare Research and Quality, 2024).
The Bottom Line
The time has come for widespread promotion and implementation of the ICU Liberation Bundle to meet the short- and long-term needs of ICU survivors, to reduce the financial and psychological burden on the families of the critically ill, and to improve resource utilization for an overburdened healthcare system.
Impact Advisors works with hundreds of leading hospitals, health systems, specialty care and physician groups to improve the quality, safety, efficiency, availability, and outcomes of clinical care.
References
Barr, J., Downs, B., Ferrell, K., Talebian, M., Robinson, S., Kolodisner, L., Kendall, H., & Holdych,, J. (2024) Improving outcomes in mechanically ventilated adult ICU patients following implementation of the ICU Liberation (ABCDEF) Bundle across a large healthcare system. Critical Care Explorations, 6(1), e1001. https://doi.org/10.1097/CCE.0000000000001001
Barr, J., Ghaferi, A.A., Costa, K. D., Hedlin, H. K., Ding, V. Y., Ross, C., Pun, B.T.,, Watson, S. R., & Asch, S.. M. (2020) Organizational characteristics associated with ICU Liberation (ABCDEF) Bundle implementation by adult ICUs in Michigan. Critical Care Explorations, 2(e0169). https://doi.org/10.1097/CCE.0000000000000169
Brown, J., Querubin, J. A., Ding, L., Mack, W., Chen-Chan, K., Perez, F., Barr, J., Pedren, C., & Cobb, J. P. (2022). Improving ABCDEF Bundle compliance and clinical outcomes in the ICU: Randomized control trial to assess the impact of performance measurement, feedback, and data literacy training. Critical Care Explorations4(4), e0679. https://doi.org/10.1097/CCE.0000000000000679
Devlin, J. W., Skrobik, Y., Gelinas, C., Needham, D. M., Slooter, A. J. C., Pandharipande, P. P., Watson, P. L., Weinhouse, G. L., Nunnally, M. E., Rochwerg, B., Balas, M. C., Boogaard, M., Bosma, K. J., Brummel, N., Chanques, G., Denehy, L., Drouot, X., Fraser, G. L.Harris, J.E., Joffe, A. M., Kho, M. E., Kress, J. P., Lanphere, J. A., McKinley, S., Neufeld, K. J., Pisani, M.A., Payen, J. F., …K., Alhazzani, W. (2018). Clinical practice guidelines for the prevention and management of pain, agitation/sedation, delirium, immobility, and sleep disruption in adult patients in the ICU. Critical Care Medicine, 46(9),e826-e873. https://doi.org/10.1097/CCM.0000000000003299
Ely, W.E. (2017) The ABCDEF Bundle: Science and philosophy of how ICU Liberation serves patients and families. Critical Care Medicine, 45(2), 321-330. https://doi.org/10.1097/CCM.0000000000002175
Fish, J. T., Baxa, J. T., Draheim, R. R., Willenborg, M. J., Mills, J. C., Sticht, L. A., Hankwitz, J. L., Wells, J. A., & Jung, H. S. (2021). Five year outcomes after implementing a pain, agitation and delirium protocol in a mixed intensive care unit. Journal of Intensive Care Medicine, 37(8). https://doi.org/10.177/08850666211063404
Hermans, G., Van Mechelen, H., Clerckx B., Vanhullenbusch, T., Mesotten, D., Wilmer, A., Casaer, M. P., Mersseman, P., Debaveye, Y., Wouters, P. J., Gosselink, R. & Van den Berghe, G. (2014) Acute and long-term outcomes of ICU-acquired weakness: A cohort study and propensity matched analysis. Crit Care, 18(1) 466. https://doi.org/1010.1186/cc13656
Milbrandt, E. B., Deppen, S., Harrison, P. L., Shintani, A. K., Speroff, T., Stiles, R. a., Truman, B., Bernard, G. R., Dittus, R. S., & Ely, W. E. (2004). Costs associated with delirium in mechanically ventilated patients. Crit Care Medicine, 32(4), 955-962. https://doi.org/10.1097/01.ccm.0000119429.16055.92
Pun, B.T., Balas, M., Barnes-Daly, M. Thompson, J. L., Barr, J., Carson, S. S.., Devlin, J. W., Engel, H. J., Esbrook, C. L., Hargett, K. D., Harmon, L., Hielsberg, C., Jackson, J. C., Kelly, T. L, Kumar, V., Millner, L., Morsem A., Perme, C. S., Posa, P. J., Puntillo, K. A., Schweikert, W. D., Stollings, J. L, Tan, A., McGowan, L., & Ely, W. E. (2018) Caring for critically ill patients with the ABCDEF bundle: Results of the ICU Liberation Collaborative in over 15,000 adults. Critical Care Medicine. https://doi.org/10.1097/CCM.0000000000003482
Shirasaki, K., Hifumi,, T., Nakanishi, NM., Nosaka, N., Miyamoto, K., Komachi, M.H., Haruna, J., Inoue, S., & Otani, N. (2023). Postintensive care syndrome family: A comprehensive review. Acute Med Surg, 11(11): e939. https://doiu.org/10.1002/ams2.939
Rawal, G., Yadav, S., & Kumar, R. (2017) Post-intensive care syndrome: An overview. Journal of Translational Internal Medicine, 5(2), 90-92. https://doi.org/1515/jtim-2016-0016
Society of Critical Care Medicine (2019, November). An interview with an ICU Liberation Collaborative Leader and Participant. https://sccm.org/Blog/November-2019/How-ICU-Liberation-Brought-Value-to-Our-Patients,#:~:text=The%20net%20effect%20of%20our,%2C%20and%20third%2Dparty%20payers.
Society of Critical Care Medicine (n.d.) ICU Liberation Bundle implementation data [Infographic] ICU Liberation https://www.sccm.org/ICULiberation/Home


