Healthcare organizations everywhere continue to grapple with financial and operational challenges and are increasingly focused on how to drive revenue improvements and decrease costs. However, initiatives focused on increasing productivity and efficiency can have negative consequences by creating a high-pressure clinical environment that exacerbates provider burnout. Organizations that are successfully driving transformational change have learned that understanding the psychological health of providers and bolstering their emotional resilience is key to delivering safe, high-quality, and efficient patient care.
Provider Burnout Increases Risk and Decreases Care Quality and Patient Satisfaction
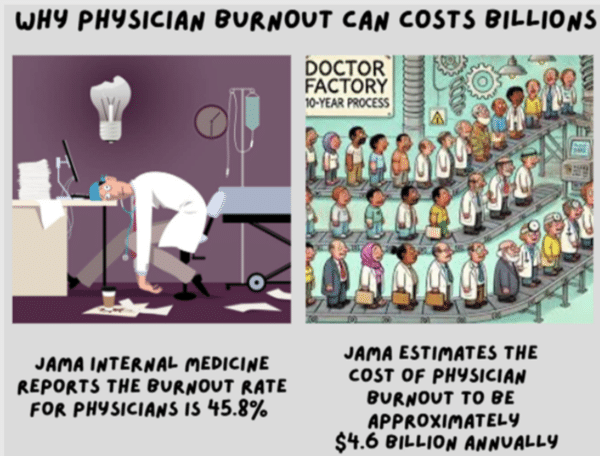
Nearly half of physicians report feeling burnt out according to the Journal of the American Medical Association (JAMA)(1). The organization’s meta-analysis, consisting of 47 studies and approximately 42,000 physicians, showed that physician burnout doubled the likelihood of patient safety risks, decreased quality of care, and decreased patient satisfaction – and physician burnout is proven to hinder overall healthcare system performance. JAMA’s study indicated a link between burnout and high rates of medical errors, poor communication with patients and staff members, and decreased empathy within the workplace.
Several individual and systemic factors contribute to the growing mental health crisis among providers. Often, providers state, “[our] clinic hasn’t been the same since COVID,” and this is true. The pandemic exacerbated key challenges within the workplace along with increased caseloads for providers, leading to a burnout rate in 2021 of 62.8%, according to a Mayo Clinic report (2). Many organizations have maintained higher productivity levels with less support staff further compounding stressors. In the eyes of a provider, working long hours, caring for more and more complex patients, providing routine crisis intervention, and increasing emphasis on documentation all contribute to a provider’s mental burden. When compromised, a physician’s clinical performance suffers, as well as their decision-making, and most importantly patient outcomes.
Performance Improvement Strategies That Also Promote Provider Wellbeing
are Key to Sustainable Success
Driving transformational change while managing provider burnout requires a balance of strategic leadership, clear communication, and a deep understanding of human wellbeing. Organizations that promote a culture of openness and foster an environment where provider and staff wellbeing is prioritized can increase satisfaction (employees and patients) and increase productivity and efficiency. Several strategies have had success in the ambulatory clinic setting.
1.) Fostering a Culture of Engagement
Engaging providers and staff in the process of identifying challenges and designing solutions engenders buy-in to the changes themselves but also demonstrates respect for their knowledge and skillset, which increases satisfaction. It also presents the opportunity to understand and gain confidence in the skills and abilities of fellow team members and potentially shift workflows to take better advantage of skill mix. Enlisting “change champions”—natural leaders who help promote changes and remove barriers among their peers—is another effective method of increasing the adoption of changes. And finally, recognizing and rewarding achievements and milestones is essential for keeping everyone engaged in continuous improvement.
2.) Flexible Scheduling and Workload Management
Establishing utilization guidelines, communication structures, and staffing controls assures adequate staff-to-patient volumes while maintaining the agility needed to address the varying complexity of patients. Leveraging flexible staffing models can improve the work-life balance of team members and the overall productivity of the clinic.
3.) Implementation of Peer Support Programs
Tactics to foster psychological safety among providers can range in investment from offering access to support via a free hotline, such as the Physician Support Line, which is run by volunteer psychiatrists for healthcare workers, to highly structured programs that are governed and operated like any formal initiative. The latter has shown positive outcomes, according to the research article, “Implementation and Effectiveness of a Physician-focused Peer Support Program” published in PLOSONE (3). The study examined the effectiveness of a Peer Outreach Support Team (POST), “a group of physician leaders and key stakeholders convened to support physicians… facing any professional stress.” POST participants, who received payment for their involvement in the program, received formal training covering “burnout, peer support, program structure, interaction components, identifying red flags, and accessing additional resources.” The cost of the program was found to be reasonable and acceptable given the negative financial impact that results from provider burnout.
The National Academy of Medicine (NAM) created the Clinician Well-Being Collaborative (4) an effort designed to raise the visibility of clinician anxiety, burnout, depression, stress, and suicide; improve baseline understanding of challenges to clinician well-being; and advance evidence-based, multidisciplinary solutions to improve patient care by caring for the caregiver. The Clinician Well-Being Collaborative convenes, publishes, and shapes the national conversation to target priority areas of leadership engagement, stop the culture of silence, and provide organizational practices and support on recommendations, and sustainability.
4.) Onsite Mindfulness and Stress Mangement Resources and Services
Often overlooked or viewed as being too extravagant or expensive, services that promote mindfulness and help employees manage stress can be affordable and effective. Establishing an agreement with a local provider for massage, yoga or mindfulness sessions can be an inexpensive investment in the wellbeing of providers and staff, who may find it easier to step away from the clinic for a 15-minute chair massage or meditation session and return to patients refreshed and more productive. In one clinic in Louisville, KY, chair massages are offered once a month for staff and doctors. It began as a one-time “thank-you” from leadership and transitioned into a monthly benefit. Staff and doctors noted how it helped them have a productive and less stressful day in the clinic. Other examples include offering helpful resources (e.g., Lyra Health provides mental health support tailored for healthcare providers) and books (e.g., The Resilient Practitioner), dedicated quiet rooms, exercise space, group meditation and yoga.
5.) Leveraging Technology to Automate Routine Tasks
EHRs have embedded tools to optimize workflows and improve communication between providers; and most EHR vendors are proactively developing more tools that leverage AI to automate administrative and other tasks that allow providers to operate at the top of their licenses.
In conclusion, fostering an environment that supports the wellbeing of providers contributes to the success of initiatives focused on increasing productivity and efficiency. By engaging providers and staff in the process, utilizing flexible scheduling and workflow management, implementing peer support programs, providing mindfulness and stress management services, and leveraging existing and new technologies, clinics can reduce the pressure on providers and teams while boosting their productivity
Impact Advisors’ physician enterprise team brings a robust combination of clinical, operations, analytics, and IT expertise to the table. This background and knowledge allow us to analyze and determine the right structure, processes, and tools to implement within your physician practice to improve provider satisfaction and help minimize burnout.