In the last two years, surveys have shown that 41% of US adults currently have some form of healthcare debt (Kaiser Family Foundation), and 38% say they or a family member have forgone or delayed medical care due to cost (Gallup). With these alarming statistics, it is no wonder that a consistent finding across consumer experience studies shows that a patient’s experience with provider billing is a particularly crucial factor in determining overall satisfaction and whether to return to the provider.
As many hospitals have resorted to cost-cutting measures and layoffs to improve their cash flow, one process change is often overlooked: Payment education for patients. Payment education for patients can have a large positive impact. According to an Apex/InfoTrends survey, 70% of patients said they would be more likely to pay their medical bill in a timely manner if they received a cost estimate on the day of their service. Furthermore, once patients leave the hospital, they are 50% less likely to pay their bill. When the right dialogue and processes between patients, providers, and hospitals take place, it can improve revenue and patient experience.
A Typical Patient Experience
Below is a sample patient experience to illustrate what typically happens and what goes wrong.
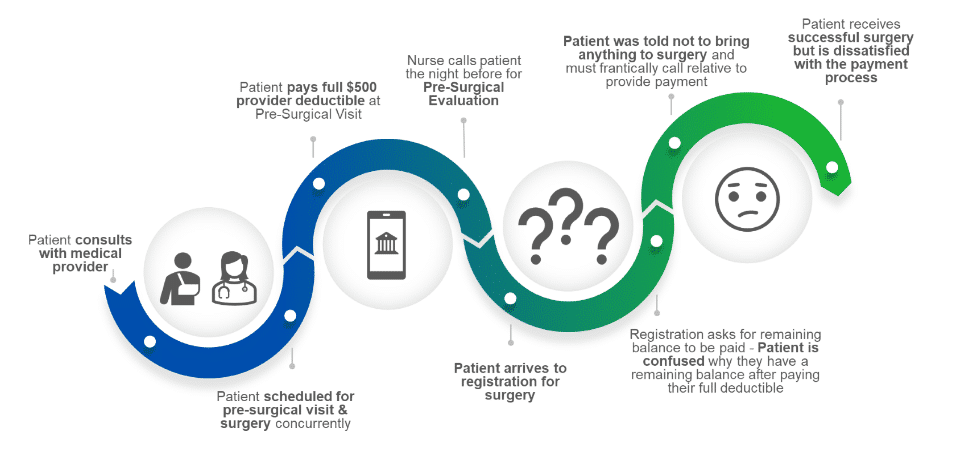
A Typical Patient Journey
- Patient scheduled for pre-surgical visit and surgery at same time.
- Patient paid full $500 of their provider deductible at pre-surgical visit.
- Patient arrived to check in for surgery and was greeted by the registration desk. Patient advised of a $1,000 balance remaining on their account and asked to pay.
- Patient informed registration they paid $500 towards their deductible at their pre-surgical visit. Patient believes they are being charged twice for their surgery.
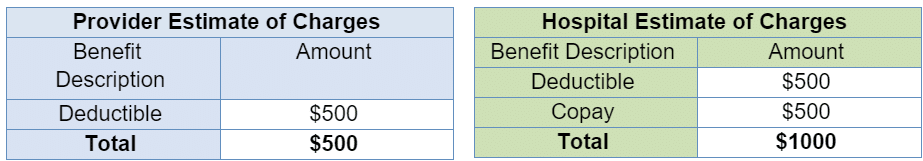
- Patient did not realize they had a hospital charge in addition to the provider charge. The hospital charge has a $500 deductible and a $500 copay, which totals $1,000.
- The patient explained they were not informed of owing any additional payment when they spoke to the nurse the night before and had been told not to bring anything with them upon arrival.
- The Registrar explained there are two bills, one for the provider and one for the hospital. The patient is frustrated before undergoing surgery.
What Went Wrong
- Patient not advised there would be two estimates - one for hospital and one for provider charges
- Patient did not understand how their insurance plan determined their cost share for their services
- Patient was not instructed to call their insurance carrier as a resource to understand the cost of upcoming services.
- Patient was not informed during the call with the nurse, prior to the visit, about any payment responsibilities they may have at the time of service
Setting Up a Successful Patient Journey
Patients need to be guided through the tangled web of healthcare, and this includes the final stage of billing insurance and collecting on patient liability. Every aspect of the patient experience should be viewed as an opportunity to ensure there is an understanding around the patient’s financial liability. Below are key areas at each stage of the patient journey to improve communication.
Pre-Visit
Technology
Encourage use of web-based tools (e.g., MyChart) to inform the patient before arrival of their balance and give them the option to pay ahead of time.
Medical Group / Provider Offices
If the patient and their provider decide hospital services are needed, the staff should advise the patient that an estimate of charges will be available once the service is scheduled.
- Utilize a Single Billing Office (SBO) to provide all charges in one invoice vs separate charges to the patient
- Set expectations for any outstanding balance due
- Expectations can include:
- Balance paid in full prior to scheduling future services
- Making a 25%-50% payment towards the outstanding balance prior to scheduling
- Setting up a monthly payment plan
Impact to your patients’ experience: Starting the conversation early and utilizing a SBO reduces patient confusion and builds their trust in the transparency of their care.
Scheduling Department
- Scheduling agents can advise the patient about payment due on or before the date of service
- Discuss estimates when scheduling services for ambulatory care, inpatient care, and outpatient services
- Educate staff on patient liability expectations, including any outstanding balances due
Impact to your system’s financial health: Accurate scheduling processes and insurance verification can prevent denials and inaccurate misinformation during the billing process and allow patients to financially plan for their upcoming medical services.
Pre-Registration
- Prior to the patient’s hospital visit, the pre-registration team should run an estimate for expected charges and notify the patient and share when payment is expected (prior to or at time of service)
- Utilize MyChart to send the estimate of charges for the patient to review
- Develop protocols for pre-registration team members to call the patient when a balance is over a certain threshold, such as $1,000
- Remind the patient of outstanding balance protocols
- Take payment over the phone, direct them to MyChart to make payment, or advise that outstanding balances and charges are due at time of registration on the day the services are rendered
- Offer the services of financial counseling if the patient mentions a financial hardship
Impact to your system’s financial health: Protocols in Pre-Registration can reduce downstream payment delays and surprise
During Visit
Registration
- Accept payments on current and outstanding charges
- Provide continuous education and scripting support, focusing on responses to requesting patient payment at the time of service
Impact to your system’s financial health: Clear understanding of the registration process reduces the amount of eligibility or registration write-offs.
Clinical Team
- Educate clinical teams on what resources, such as MyChart or financial counseling, to direct patients to when they ask questions about costs or payments
- This includes advising the patient that full payment is due prior to or on the day of their scheduled visit. Patients should be instructed to bring a form of payment with them at time of check in, view MyChart, or call customer service to make payment or set up a payment plan
- Discharge paperwork should include past due balances and current charges to review at home
Impact to your patients’ experience: Providing your clinical team with resources & contact information can help your patients feel less anxious and prevent miscommunications about their financial liability.
Post-Visit
Technology
- The EHR system plays an influential role in patients’ experiences (or frustrations). For health systems on Epic, the hospital and provider charges can be combined into one consolidated bill for the patient
- Combine both hospital and provider charges into one system
- Provide scripting for all staff to explain the billing process and eliminate confusion
- Post-visit communications (text messages, emails) should thank the patient for their visit and remind them of upcoming balances, how to pay, and what to expect
- MyChart is the most effective way to push balance notifications to patients
Impact to your system’s financial health: Accurate workflows built within your EHR ensures your hospital is billing and collecting accurately. Clarifying your technology processes can save hundreds of hours of rework, working denials, contacting dissatisfied patients, and other time-consuming back-end tasks.
Customer Service / Billing Department
- If the patient does not pay at the time of service, the hospital’s billing department should follow up with the patient and provide clarity on the balance due
- The billing department should be able to set up payment plans when necessary and follow up via call, account alert, email, text, or MyChart
Impact to your patients’ experience: After your patient has received care, a trustworthy and helpful Customer Service department can make or break their overall impression of their experience at your health system.
Carefully reviewing all the areas in the patient journey within your organization where patient liability can be discussed will improve both your bottom line and your patient experience. Impact Advisors can help with patient balance and POS collections.
Related reading:


