
Hospital-at-Home Background and Core Components
As virtual care continues to evolve and is now a staple of care delivery, the hospital-at-home, a hybrid virtual / in-person care model where inpatient level services are provided in a patient’s home, is transforming care. The concept is by no means new, but interest in developing formal hospital-at-home initiatives was rekindled during the pandemic as a way to alleviate capacity issues while also limiting transmission of the virus. The launch of CMS’ Acute Hospital Care at Home program in 2020 allowed providers to apply for waivers of the requirement for “nursing services to be provided on premises 24 hours a day, 7 days a week.” The program was recently extended through the end of 2024. As of 4/27/23, there were 124 health systems (representing 278 hospitals) in 37 states that had been approved for a waiver.
It is important to note the “hospital-at-home” is a concept whereas “Acute Hospital Care at Home” is a specific program from CMS that allows providers to receive reimbursement for delivering inpatient level care in a Medicare beneficiary’s home. The hospital-at-home concept has been around for decades – and there are many hospital-at-home initiatives underway today that significantly pre-date the pandemic. Given that reimbursement has long been the biggest barrier to scaling hospital-at-home initiatives, the launch – and subsequent extension – of CMS’ program was a logical catalyst in terms of generating more interest among providers. But the hospital-at-home is much broader than the program from CMS – and many of the organizations who implemented a hospital-at-home to care for COVID patients are now looking to build on their experience and expand.
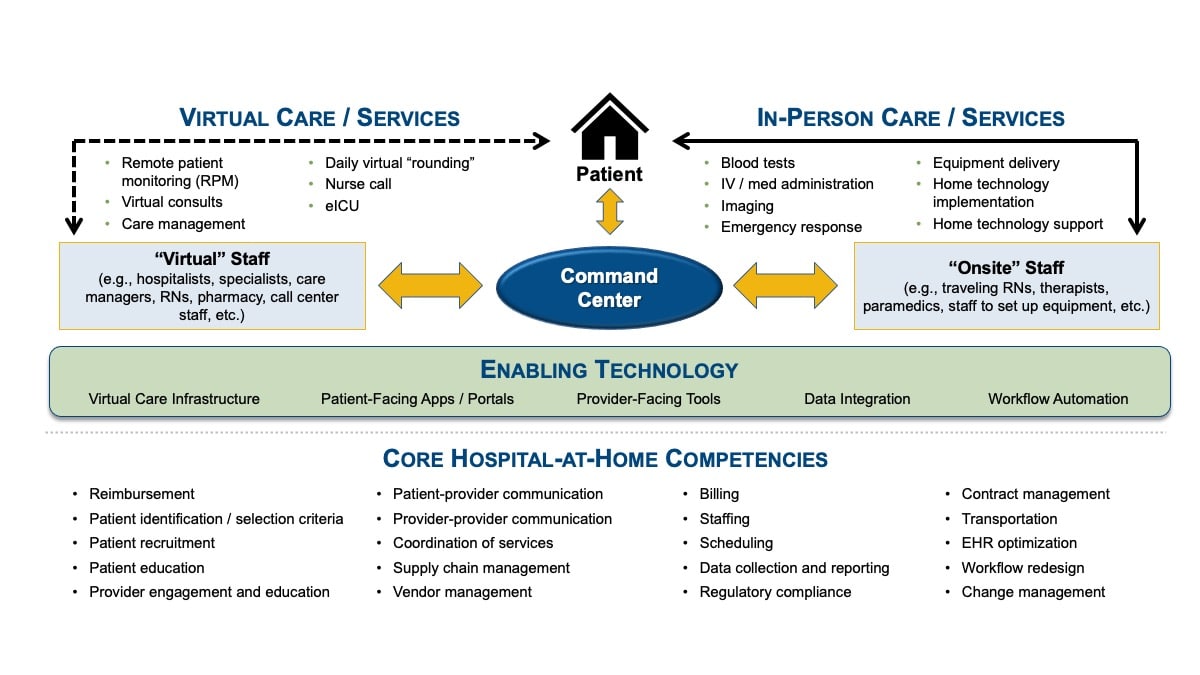
While each hospital-at-home will inherently be somewhat different, there are three essential components for any initiative.
- They hybrid combination of virtual and in-person services offered
- A command center and the enabling technology
- The underlying core competencies needed for success
Hospital-at-Home Framework
Five Questions to Ask
Although the hospital-at-home has generated considerable interest among providers, the reality is the model is not a fit for every health system. There are five key questions that any provider organization should carefully consider before moving deciding to move forward with a hospital-at-home initiative:
1. Do we have a problem that a hospital-at-home could solve?
2. Is a hospital-at-home feasible in our market?
3. Do we understand the reimbursement?
4. Do we have enough of the right experience?
Even health systems with significant experience in the underlying core competencies required for a hospital-at-home will still likely need to strategically position partners and capabilities to enhance their offerings. This is especially true as needs change when trying to get the initiative to scale.
5. Have we fully assessed our existing virtual care processes, capabilities, and controls?
As a result, before launching a hospital-at-home – or any new initiative with a virtual care component – health systems need to carefully review their current telehealth processes, capabilities, and controls for billing compliance (e.g., coding, documentation, and licensing / telehealth registrations).
The Bottom Line
Anything other than a resounding “yes” to the five questions above should give a health system pause before embarking on efforts to build a hospital-at-home. However, just because the hospital-at-home isn’t a fit for your health system doesn’t mean the model is not something to consider in the future, especially as reimbursement evolves, your needs change, and industry experience with the concept becomes more widespread.
The hospital-at-home ultimately represents just one type of care model that involves virtual care. There may be other virtual care initiatives (and even other hybrid virtual / in-person initiatives) worth pursing that are more closely aligned with your organization’s unique strategic priorities and which represent a better fit for the realities in your market. However, before moving forward with any new initiative with a significant virtual care component – or even before expanding on existing virtual care offerings – it is essential that your health system has a plan in place to understand and refine your existing telehealth processes, capabilities, and controls.


