Achieving Sustainable Margin Results with an “Operations and Capacity Center” (OCC)

Many hospitals and health systems face capacity challenges that prohibit them from caring for patients in their communities. These challenges are due to multifaceted factors, including ongoing staffing shortages, siloed processes, and the inability to use technology for real-time information and monitoring. Implementing an operations and capacity center (OCC) – or expanding on existing OCC capabilities – can help your organization increase capacity, optimize patient throughput, and achieve sustainable margin results. However, success hinges on embracing a combination of operational and cultural changes.
What is an Operations and Capacity Center?
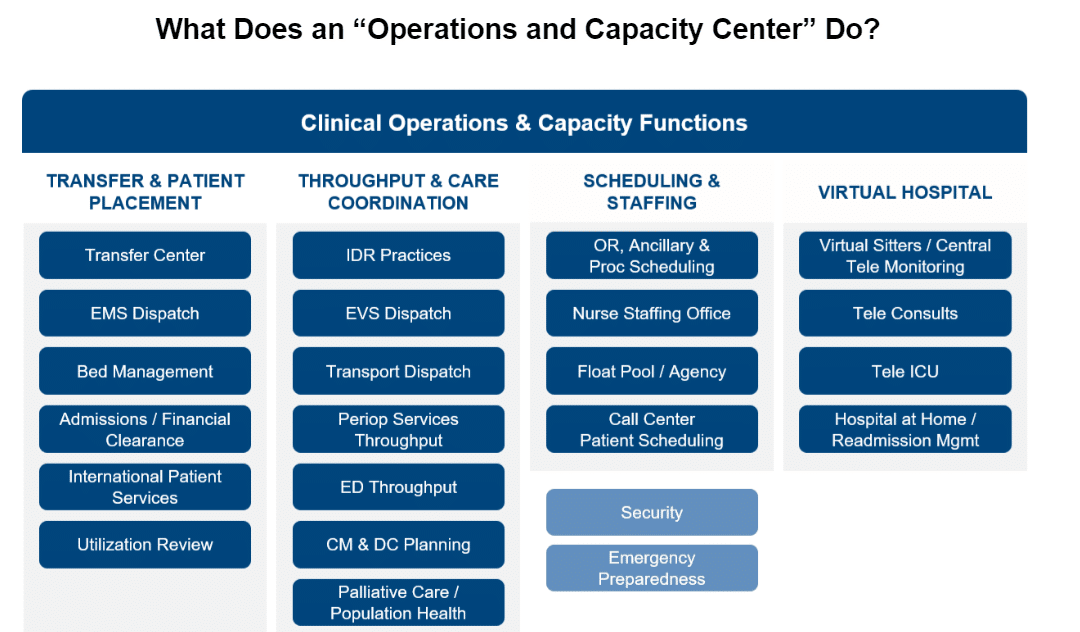
An operations and capacity center (OCC) can have a variety of “labels,” such as Mission Control, Command Center, or Patient Logistics Center, to name a few. Ultimately, an OCC is more about the function and not the name. In most cases, an OCC is a centralized department responsible for overseeing and optimizing the use of your hospital or health system’s resources to ensure that patient care is delivered efficiently and effectively. The primary focus of any OCC is to:
- Manage the hospital or health system’s resources, including beds, staff, equipment, and other critical resources to optimize capacity;
- Avoid bottlenecks and/or access to patient care;
- Reduce patient wait times; and
- Improve overall patient flow through the hospital or health system while providing quality care
“Centralized” doesn’t necessarily mean a single physical location, but vital components of a well-functioning OCC are the centralization of leadership functions and strong strategy and governance, especially given the growing prevalence of remote resources and virtual health programs.
An OCC should be aligned with the organization’s overall strategic plan to be most effective. This strategy will guide the formation and evolution of an OCC. Equally important, an OCC should leverage the use of technology, both existing technology investments and the consideration of new technologies.
Success Requires Operational and Cultural Change
There are important operational and cultural elements to consider when developing the plan for a new OCC or expanding on existing OCC capabilities. A critical part of achieving sustainable margin results from an OCC is how your organization standardizes operational processes and closes gaps in high-impact workflows. For example, the methods of how patients access and move through the healthcare continuum can vary from hospital to hospital, even within the same healthcare system. The “gaps” in processes or varying use of technology can increase patient wait times and even lead to patients leaving the system for an alternative location (i.e., a competitor) for care. Thus, examining each process and workflow is essential in planning for or expanding the capabilities of an OCC.
The cultural pieces are just as crucial, such as communicating a burning platform for change across the enterprise and securing engaged sponsorship from executives and physicians. During the communication campaign, it is essential to promote awareness that the OCC is not a physical space but rather a hub of real-time information and action under a unified leadership structure.
How to Get Started
Critical steps for any hospital or health system to achieve long-term results and continuous improvement from an OCC include:
1.) Defining success metrics and targets
There is a significant amount of data and KPIs that help drive the performance of an OCC – and any success metrics your organization defines must be closely aligned with your strategic plan. Overall, there are two types of OCC success metrics. First are the retrospective “scorecard” measures that track your baseline performance and progress against your goals. These are typically looked at monthly or quarterly and used to make longer-term operational decisions. The second type of metrics is real-time analytics, which can help your organization understand day-to-day barriers and drive action in the moment. To utilize these most effectively, real-time metrics are often displayed within the physical space of the OCC as well as on desktops to support specific team members and functions.
While data is available, it is only as valuable as what you do with it. For example, if you are seeing a discharge delay, you must have a corresponding process, downstream workflow, and awareness across the enterprise of what action needs to be taken – and who is accountable for taking that action.
2.) Establishing system-level leadership and governance
The foundation of a successful OCC governance model requires integration between multiple key stakeholders, including executive leadership, providers, quality committees, and department-level operational teams. All team members impacted by the workflows of the OCC must be engaged to ensure cost-effective operations and standardized practices across your health system. This governance structure will ensure alignment with system strategies and serve as oversight for processes, metrics, and roadblocks.
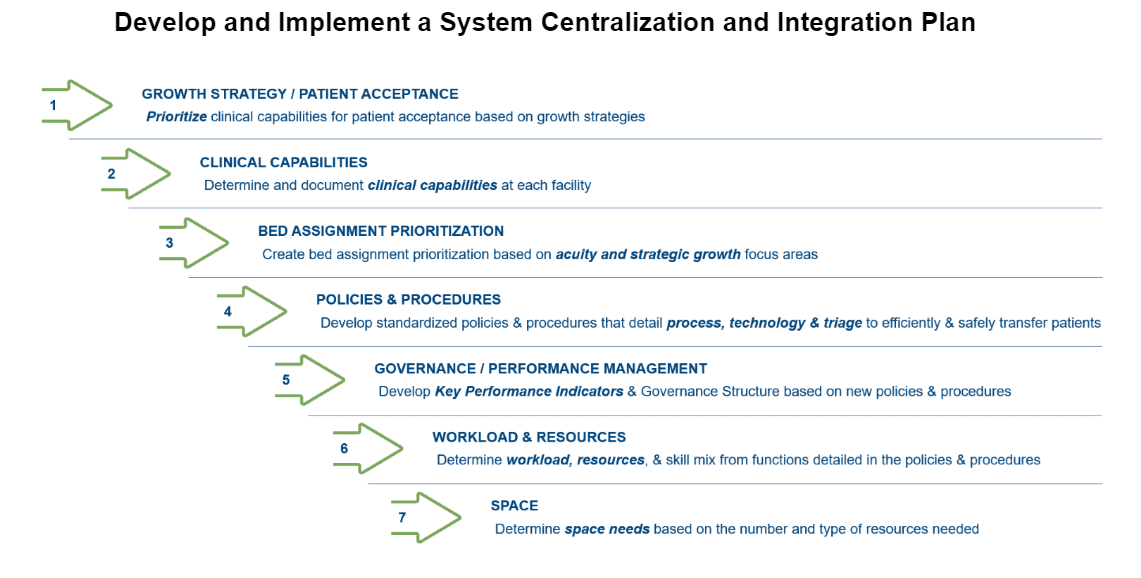
3.) Standardizing processes across the health system
To promote efficient, cost-effective care and achieve sustainable financial outcomes from an OCC, there should be a transition from hospital-specific centers to a comprehensive, system-wide approach. The ability to standardize processes across the enterprise – and do it effectively – is paramount. Patients should experience the same high efficiency and quality care regardless of their portal of entry into the system.
4.) Measuring financial impact
Funding a new OCC, or expanding an existing OCC, can be challenging. However, there is substantial financial benefit to be gained through these efforts. Achieving sustainable margin improvement hinges on continuously measuring the financial impact of the OCC. Efforts to manage and unlock hidden capacity will drive financial benefits in one of two ways: 1) cost avoidance by reducing excess days and 2) revenue enhancement by adding patient volume.
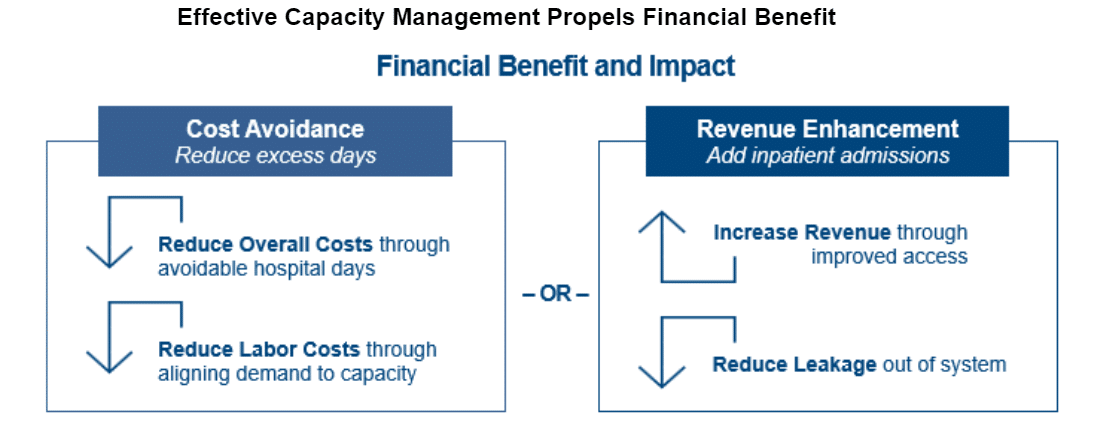
Additionally, performance improvement workstreams can complement the OCC and produce additional financial benefits, allowing the hospital system to continue meeting patient needs and financial goals.
Benefit Beyond Margin Improvement
In addition to the financial benefits of an OCC, the impact on quality is evident through the improvement of patient care processes, standardization, evidenced-based care pathways, and reduction of patient wait times. Ensure your organization gets credit for the improved quality of care and optimized patient experience by preparing your quality team for an increased focus on clinical documentation. When your OCC is optimized, it is more important than ever for your clinicians to have the tools they need to document the accurate acuity of your inpatient population. Documentation-sensitive quality measures significantly impact many of the large national quality ranking systems such as CMS Star Scores, Leapfrog Grades, and U.S. News Rankings.
Three ways you can ensure the success of your quality programs while increasing speed to value for your OCC initiatives are:
- Create reporting tools for Quality Benchmarking that allow you to compare your hospitals and specialties against other similar peer groups and quickly identify areas of opportunity;
- Build workflow tools into your Electronic Health Record (EHR) that make it easy for providers and clinical documentation team members to quickly identify and fix any documentation gaps in patient charts that will negatively impact quality scores; and
- Develop real-time quality process metric dashboards that allow you to forecast quality score performance before scores are published to the public.
Focusing on these three key initiatives will set your organization up for long-term success and market differentiation. The benefits of a best-in-class OCC extend far beyond financial performance, and long-term success is guaranteed when you are focused on creating a strong foundation dedicated to quality outcomes.
The Bottom Line
An operations and capacity center (OCC) can help your hospital or health system overcome barriers related to operational efficiency. However, success depends on laying the right foundation from the beginning and embracing operational and cultural changes.
Impact Advisors can help your organization enhance care delivery. We work with hundreds of leading hospitals, health systems, specialty care, and physician groups to improve the quality, safety, efficiency, availability, and outcomes of clinical care.
























